Stanya-Shodhana Mahakashaya - A Potential Solution for Diseases in Breast Feeding Infants - A Review
DOI:
https://doi.org/10.21760/jaims.10.4.17Keywords:
Sthanya, Breast Milk, Stanyashodhan Mahakashaya, purification of breast milk, AyurvedaAbstract
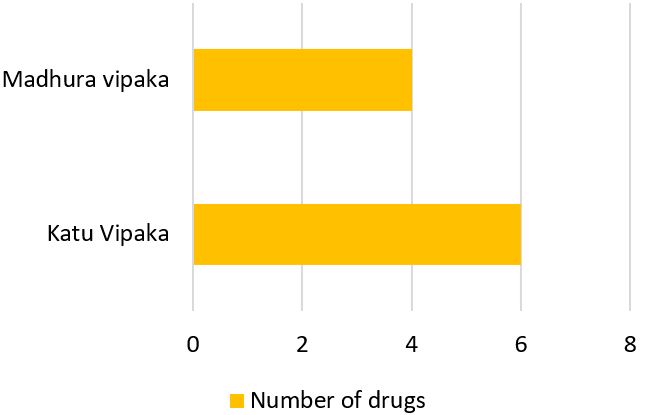
Breast milk is referred as Stanya in Ayurveda texts also known as Piyush (nectar/Amrita); justifies totally with its importance for a newborn. Newborns primarily rely on the breast milk for their nutrition. Ayurvedic texts have described qualities of normal breast milk under the heading “Shuddha Stanya”. Emphasis has been given on the aspect of abnormalities of breast milk and their consequences on infants and as well as on mothers in Ayurveda classics. Vitiation in the normal qualities of Stanya is described as Stanya Dushti. To deal with the same, a concept of Stanyashodhan is mentioned in Charak Samhita in the form of group of ten drugs known as Stanyashodhan Mahakashaya. This article involves synthesizing information from various Ayurvedic texts and internet databases like PubMed, PubMed Central Databases, Google Scholar, CrossRef to substantiate the Stanya Shodhan attributes of these herbs. Neonates are highly susceptible to medication errors and adverse drug events due to their fragile physiology, immature organ systems, and limited ability to metabolize and eliminate medications. This problem can be solved if we treat the mother and thus providing treatment to infants through the Shodhita breast milk using Stanyashodhana Mahakashaya.
Downloads
References
Ballard O, Morrow A. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. 2013 Feb;60(1):49-74.
Lynos KE, et al. Breast milk, a source of beneficial microbes and associated benefits for infant health. Nutrients. 2020 Apr 9;12(4):1039. doi: 10.3390/nu12041039. PMID: 32283875; PMCID: PMC7231147.
AlThuneyyan DA, et al. The effect of breastfeeding on intelligence quotient and social intelligence among seven- to nine-year-old girls: a pilot study. Front Nutr. 2022 Feb 18;9:726042. doi: 10.3389/fnut.2022.726042. PMID: 35252287; PMCID: PMC8894195.
Kashyapa Samhita by Vrddha Jivaka, with Sanskrit introduction by Pandit Hemaraja Sharma and Vidyotini Hindi commentary by Srisatyapal Bhisagacharya. Varanasi: Chaukhambha Sanskrit Sansthan; 2013. Sutrasthana, chapter 19.
Charaka Samhita of Agnivesa, with Hindi commentary by Kasinatha Sastri. Varanasi: Chaukhambha Sanskrit Sansthan; 2012. Sharirasthana C.Sh. 8/54. p. 848.
Yi DY, Kim SY. Human breast milk composition and function in human health: from nutritional components to microbiome and microRNAs. Nutrients. 2021;13(9):3094. doi: 10.3390/nu13093094.
Yi DY, Kim SY. Human breast milk composition and function in human health: from nutritional components to microbiome and microRNAs. Nutrients. 2021;13(9):3094. doi: 10.3390/nu13093094.
Mosca F, Giannì ML. Human milk: composition and health benefits. La Pediatria Med Chir. 2017;39(2):155. doi: 10.4081/pmc.2017.155.
Kim SY, Yi DY. Components of human breast milk: from macronutrient to microbiome and microRNA. Clin Exp Pediatr. 2020;63(8):301-9. doi: 10.3345/cep.2020.00059.
Melekoglu E, et al. The impact of the human milk microbiota in the prevention of disease and infant health. Breastfeed Med. 2023 Jun 1;18(6):413-30.
Melekoglu E, et al. The impact of the human milk microbiota in the prevention of disease and infant health. Breastfeed Med. 2023 Jun 1;18(6):413-30.
Davis EC, Castagna VP, Sela DA, et al. Gut microbiome and breast-feeding: implications for early immune development. J Allergy Clin Immunol. 2022;150(3):523-34.
Charaka Samhita of Agnivesa, with Hindi commentary by Kasinatha Sastri. Varanasi: Chaukhambha Sanskrit Sansthan; 2012. Chikitsasthana chapter 30/236.
Ashtanga Samgraha of Vagbhata, with English translation by Prof. KR Srikantha Murthy. Varanasi: Chaukhambha Orientalia; Uttar Tantra chapter 1/22.
Ashtanga Samgraha of Vagbhata, with English translation by Prof. KR Srikantha Murthy. Varanasi: Chaukhambha Orientalia; Uttar Tantra chapter 2/20-22.
Ashtanga Samgraha of Vagbhata, with English translation by Prof. KR Srikantha Murthy. Varanasi: Chaukhambha Orientalia; Uttar Tantra chapter 1/23.
Ayurveda Pharmacopoeia of India. Part I, Volume I, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 92.
Ayurveda Pharmacopoeia of India. Part I, Volume I, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 103.
Ayurveda Pharmacopoeia of India. Part I, Volume IV, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 23.
Ayurveda Pharmacopoeia of India. Part I, Volume III, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 129.
Ayurveda Pharmacopoeia of India. Part I, Volume III, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 67.
Ayurveda Pharmacopoeia of India. Part I, Volume I, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 41.
Ayurveda Pharmacopoeia of India. Part I, Volume I, First Edition. Chapter MoHFW, Dept. of Ayush; 2008.
Ayurveda Pharmacopoeia of India. Part I, Volume I, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 71.
Ayurveda Pharmacopoeia of India. Part I, Volume II, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 85.
Ayurveda Pharmacopoeia of India. Part I, Volume I, First Edition. Chapter MoHFW, Dept. of Ayush; 2008. p. 107.
Antoun MD, Ramos Z, Vazques J, Oquendo I, Proctor GR, Gerena G, Franzblau S. Evaluation of the flora of Puerto Rico for in vitro antiplasmodial and antimycobacterial activities. Phytother Res. 2001;15:638-42.
Singh A, Duggal S, Singh J, Katekhaye S. An inside preview of ethnopharmacology of Cissampelos pareira Linn. Int J Biol Tech. 2010;2:57-63.
Piero NM, Eliud NM, Susan KN, et al. In vivo antidiabetic activity and safety in rats of traditionally used C. pareira in the management of diabetes mellitus in Embu country, Kenya. J Drug Metab Toxicol. 2015;6(3).
Amresh RG, Dayanand, Rao CV. Ethnomedical value of Cissampelos pareira extract in experimentally induced diarrhea. Acta Pharm. 2004;54(1):27-35.
Gul MZ, Chandrasekaran S, Bhat MY, et al. Antioxidant and enzyme inhibitory activities of Cissampelos pareira L. Ann Phytomed. 2016;5:91-8.
Nile SH, Park SW. Chromatographic analysis, antioxidant, anti-inflammatory, and xanthine oxidase inhibitory activities of ginger extracts and its reference compounds. Ind Crops Prod. 2015;70:238-44. doi: 10.1016/j.indcrop.2015.03.033.
Zhang M, Viennois E, Prasad M, et al. Edible ginger-derived nanoparticles: A novel therapeutic approach for the prevention and treatment of inflammatory bowel disease and colitis-associated cancer. Biomaterials. 2016;101:321-40. doi: 10.1016/j.biomaterials.2016.06.018.
Kumar NV, Murthy PS, Manjunatha JR, Bettadaiah BK. Synthesis and quorum sensing inhibitory activity of key phenolic compounds of ginger and their derivatives. Food Chem. 2014;159:451-7. doi: 10.1016/j.foodchem.2014.03.039.
Citronberg J, Bostick R, Ahearn T, et al. Effects of ginger supplementation on cell-cycle biomarkers in the normal-appearing colonic mucosa of patients at increased risk for colorectal cancer: Results from a pilot, randomized, and controlled trial. Cancer Prev Res. 2013;6:271-81. doi: 10.1158/1940-6207.CAPR-12-0327.
Akinyemi AJ, Thome GR, Morsch VM, et al. Effect of dietary supplementation of ginger and turmeric rhizomes on angiotensin-1 converting enzyme (ACE) and arginase activities in L-NAME induced hypertensive rats. J Funct Foods. 2015;17:792-801. doi: 10.1016/j.jff.2015.06.011.
Suk S, Kwon GT, Lee E, et al. Gingerenone A, a polyphenol present in ginger, suppresses obesity and adipose tissue inflammation in high-fat diet-fed mice. Mol Nutr Food Res. 2017;61:1700139. doi: 10.1002/mnfr.201700139.
Wei C, Tsai Y, Korinek M, et al. 6-Paradol and 6-shogaol, the pungent compounds of ginger, promote glucose utilization in adipocytes and myotubes, and 6-paradol reduces blood glucose in high-fat diet-fed mice. Int J Mol Sci. 2017;18:168. doi: 10.3390/ijms18010168.
Patel RB. Antibacterial evaluation of ethanolic extract of Cedrus deodara wood. Arch Appl Sci Res. 2010;2:179-83.
Singh D, Aggarwal SK. Insecticidal principles of Himalayan Cedar Wood Oil. J Chem Ecol. 1988;14:1145-51.
Gautam R, Saklani A, Jachak SM. Indian medicinal plants as a source of antimycobacterial agents. J Ethnopharmacol. 2007;110:200-34.
Pandey S, Devmurari V, Goyani M, Vaghani S, Jaganathan K. Formulation and evaluation of Cedrus deodara Loud extract. Int J Chem Tech Res. 2009;1:1145-52.
Halliwell B, Gutteridge JMC. Free radicals in biology and medicine. Oxford: Clarendon Press; 1989. p. 96-8.
Kar K, Puri VN, Patnaik GK, Sur RN, Dhawan BN, Kulshrestha DK, Rastogi RP. Spasmolytic constituents of Cedrus deodara (Roxb.) Loud: Pharmacological evaluation of himachalol. J Pharm Sci. 1975;64:258-62.
Winter CA, Risley EA, Nuss GW. Carrageenin-induced oedema in hind paw of rats: An assay for anti-inflammatory drugs. Proc Soc Exp Biol Med. 1962;3:544-54.
Das B, Pal D, Haldar A. A review on Cyperus rotundus as a tremendous source of pharmacologically active herbal medicine. Int J Green Pharm. 2015;9(4):198-203.
Gupta M, Banerjee D. Studies of anti-inflammatory, antipyretic, and analgesic effects of aqueous extract of traditional herbs. Indian J Pharmacol. 2013;4(4):113-20.
Nima ZA, Jabier MS, Wagi RI, Hussain HA. Extraction, identification, and antibacterial activity of Cyperus oil from Iraqi C. rotundus. Eng Technol. 2008;26:1156-9.
Sharma A, Singh N, Bharadwaj R. Ethno-pharmacotherapeutic activities of Cyperus rotundus. Int J Med Aromatic Sci. 2016;3(2):186-94.
Gupta MB, Palit TK, Singh N, Bhargava KP. Pharmacological studies to isolate the active constituents from Cyperus rotundus possessing anti-inflammatory, antipyretic, and analgesic activities. Indian J Med Res. 1971;59:76-82.
Zhang Y, Zhang Y. Marsdenia tenacissima extract inhibits proliferation and promotes apoptosis in human ovarian cancer cells. Med Sci Monit. 2018;24:6289-97. doi: 10.12659/MSM.909726.
Jana VR, Chattopadhyay N, Shw BP. Preliminary studies on anti-inflammatory activity of Zingiber officinale, Vitex negundo, and Tinospora cordifolia in albino rats. Indian J Pharmacol. 1999;31(3):232-3.
Thippeswamy G, Salimath BP. Induction of caspase-3 activated DNase-mediated apoptosis by hexane fraction of Tinospora cordifolia in EAT cells. Environ Toxicol Pharmacol. 2007;23(2):212-20.
Manjreker PN, Jolly CI, Narayanan S. Comparative studies of immunomodulatory activity of Tinospora cordifolia and T. sinensis. Fitoterapia. 2000;71(3):254-7.
Sudha P, Zinjarde S, Bhargava SY, Kumar AR. Potent α-amylase inhibitory activity of Indian Ayurvedic medicinal plants. BMC Complement Med Ther. 2011;11:1-10.
Jeyachandran R, Xavier TF, SP. Antibacterial activity of stem extracts of Tinospora cordifolia (Willd) Hook. Anc Sci Life Res. 2003;23(1):40-3.
Kapur P, Jarry H, Wuttke W, Pereira BMJ, Wuttke DS. Evaluation of the anti-osteoporotic potential of Tinospora cordifolia in female rats. Maturitas. 2008;59(4):329-38.
Shanbhag U, Kumar K, Kumar, Mishra MS. Tinospora cordifolia (Wild.) Hook. F. & Thoms. (Guduchi): Validation of the Ayurvedic pharmacology through experimental and clinical studies. Int J Ayurveda Res. 2010;1:112-21.
Sharma V, Pandey D. Protective role of Tinospora cordifolia against lead-induced hepatotoxicity. Toxicol Int. 2010;17(1):12-7.
Mary NK, Babu BH, Padikkala J. Antiatherogenic effect of Caps HT2, a herbal Ayurvedic medicine formulation. Phytomedicine. 2003;10(6-7):474-82.
Sheikh Y, Manral MS, Kathait V, Prasar B, Kumar R, Sahu RK. Computation of in vivo antidiabetic activity of Holarrhena antidysenterica seed extracts in Streptozotocin-induced diabetic rats. Iran J Pharm Ther. 2016;14:22-7.
Verma G, Dua VK, Agarwal DD, Atul PK. Anti-malarial activity of Holarrhena antidysenterica and Viola canescens, plants traditionally used against malaria in the Garhwal region of North-West Himalaya. Malar J. 2011;10:20. doi: 10.1186/1475-2875-10-20.
Daswani PG, Birdi TJ, Antarkar DS, Antia NH. Investigation of antidiarrhoeal activity of Holarrhena antidysenterica. Int J Pharm Res. 2012;164-7.
Ganapathy PS, Ramachandra YL, Rai SP. In vitro antioxidant activity of Holarrhena antidysenterica Wall. methanolic leaf extract. J Basic Clin Pharm. 2011;2:175-8.
Sharma V, Hussain S, Bakshi M, Bhat N, Saxena AK. In vitro cytotoxic activity of leaf extracts of Holarrhena antidysenterica against human cancer cell lines. Indian J Biochem Biophys. 2014;51:46-51.
Verma H, Patil PR, Kolhapure RM, Gopalkrishna V. Antiviral activity of Swertia chirata extract against herpes simplex viruses: A study by in-vitro and molecular approach. Indian J Med Microbiol. 2008;26:322-6. doi: 10.4103/0255-0857.43561.
Alam KD, Ali MS, Parvin S, Mahjabeen S, Akbar MA, Ahamed R. In vitro antimicrobial activities of different fractions of Swertia chirata ethanolic extract. Pak J Biol Sci. 2009;12:1334-7. doi: 10.3923/pjbs.2009.1334.1337.
Stuppner H, Dorsch W, Wagner H, Gropp M, Kepler P. Antiasthmatic effects of Picrorhiza kurrooa: Inhibition of allergen- and PAF-induced bronchial obstruction in guinea pigs by androsin, apocynin, and related compounds. Planta Med. 1991;57:A62. doi: 10.1055/s-2006-960324.
Win NN, Kodama T, Lae KZW, Win YY, Ngwe H, Abe I, Morita H. Bis-iridoid and iridoid glycosides: Viral protein R inhibitors from Picrorhiza kurroa collected in Myanmar. Fitoterapia. 2019;134:101-7. doi: 10.1016/j.fitote.2019.02.016.
Joy KL, Kuttan R. Anti-diabetic activity of Picrorhiza kurroa extract. J Ethnopharmacol. 1999;67:143-8. doi: 10.1016/S0378-8741(98)00243-8.
Gaddipati JP, Madhavan S, Sidhu GS, Singh AK, Seth P, Maheshwari RK. Picroliv—A natural product protects cells and regulates gene expression during hypoxia/reoxygenation. Mol Cell Biochem. 1999;194:271-81. doi: 10.1023/A:1006982028460.
Rajkumar V, Guha G, Ashok Kumar R. Antioxidant and anti-neoplastic activities of Picrorhiza kurroa extracts. Food Chem Toxicol. 2011;49:363-9. doi: 10.1016/j.fct.2010.11.009.
Dwivedi Y, Rastogi R, Garg NK, Dhawan BN. Picroliv and its components kutkoside and picroside I protect liver against galactosamine-induced damage in rats. Pharmacol Toxicol. 1992;71:383-7. doi: 10.1111/j.1600-0773.1992.tb00566.x.
Engels F, Renirie BF, Hart BA, Labadie RP, Nijkamp FP. Effects of apocynin, a drug isolated from the roots of Picrorhiza kurroa, on arachidonic acid metabolism. FEBS Lett. 1992;305:254-6. doi: 10.1016/0014-5793(92)80680-F.
Lee HS, Ahn HC, Ku SK. Hypolipemic effect of water extracts of Picrorhiza rhizoma in PX-407 induced hyperlipemic ICR mouse model with hepatoprotective effects: A prevention study. J Ethnopharmacol. 2006;105:380-6. doi: 10.1016/j.jep.2005.11.010.
Verma PR, Joharapurkar AA, Chatpalliwar VA, Asnani AJ. Antinociceptive activity of alcoholic extract of Hemidesmus indicus R. Br. in mice. J Ethnopharmacol. 2005;102(2):298-301.
Baheti JR, Goyal RK, Shah GB. Hepatoprotective activity of Hemidesmus indicus R. Br. in rats. Indian J Exp Biol. 2006;44(5):399-402.
Mehta A, Sethiya NK, Mehta C, Shah GB. Anti-arthritis activity of roots of Hemidesmus indicus R. Br. (Anantmul) in rats. Asian Pac J Trop Med. 2012;5(2):130-5.
Anoop A, Jegadeesan M. Biochemical studies on the anti-ulcerogenic potential of Hemidesmus indicus R. Br. var. indicus. J Ethnopharmacol. 2003;84(2-3):149-56.
Ravishankara MN, Shrivastava N, Padh H, Rajani M. Evaluation of antioxidant properties of root bark of Hemidesmus indicus R. Br. (Anantmul). Phytomedicine. 2002;9(2):153-60.
Mary NK, Achuthan CR, Babu BH, Padikkala J. In vitro antioxidant and antithrombotic activity of Hemidesmus indicus (L) R. Br. J Ethnopharmacol. 2003 Aug 1;87(2-3):187-91.
Kotnis MS, Patel P, Menon SN, Sane RT. Renoprotective effect of Hemidesmus indicus, a herbal drug used in gentamicin-induced renal toxicity. Nephrology. 2004 Jun;9(3):142-52.
Gayathri M, Kannabiran K. Hypoglycemic activity of Hemidesmus indicus R. Br. on streptozotocin-induced diabetic rats. Int J Diabetes Dev Ctries. 2008 Jan;28(1):6.
Charaka Samhita. Sutrasthana chapter 26.
Dixit N, Choudhary P. Role of Stanya Shodhana Mahakashya in the treatment of Stanyadushti—A case report. J Ayurveda Integr Med Sci. 2023;9:183-6. doi: 10.21760/jaims.8.9.30.