Role of Khadira-Triphaladi Kashaya in the management of Plaque Psoriasis: A Review
DOI:
https://doi.org/10.21760/jaims.10.4.37Keywords:
Ayurveda, Herbs, Kustha, Plaque Psoriasis, Skin disorderAbstract
Background: Globally, the prevalence of psoriasis ranges from 0.09% to 11.4%. It is found to be between 1.5% and 5% in the majority of developed nations. In India, its prevalence rate varies between 0.44 and 2.8%. It is an autoimmune noninfectious, chronic, inflammatory skin disorder where altered keratinization of epidermal cell takes place with well-defined erythematous lesion and silvery plaques. In Ayurveda, according to sign and symptoms of psoriasis we can correlate it with Kapha and Pitta dominant Tridoshaja Kustha. Extensive research work has been conducted on psoriasis, yet a cost-effective and palatable cure remains elusive.
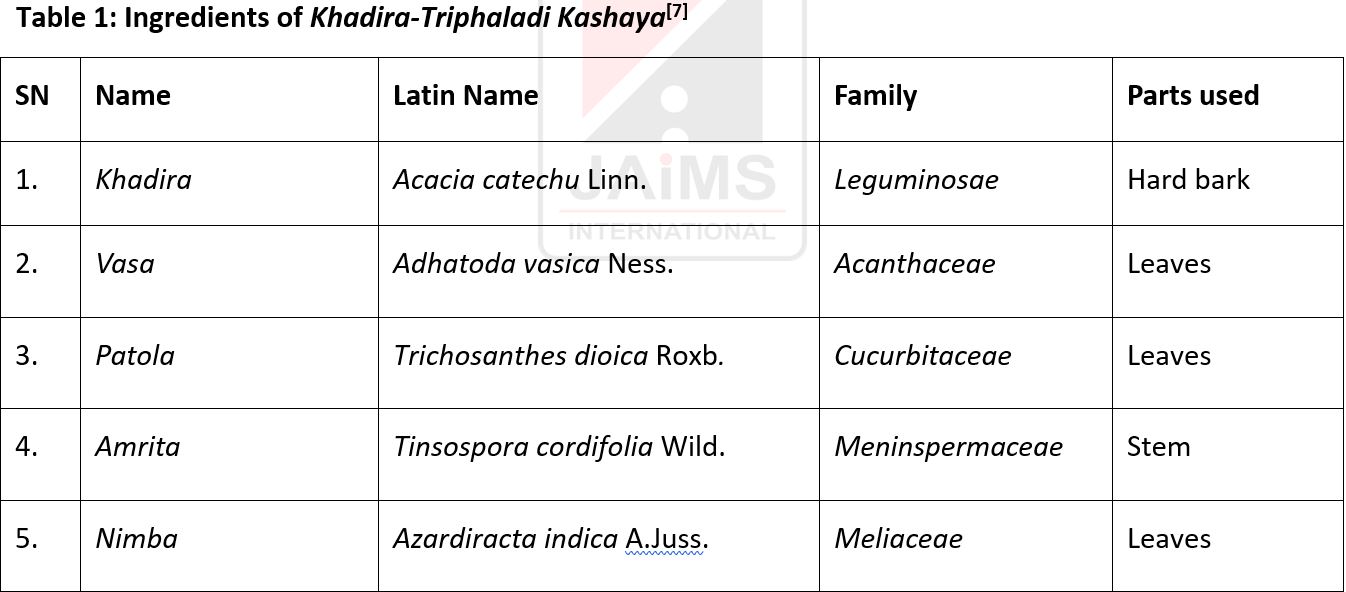
Materials and Methoda: The review on effect of Khadira-Triphaladi Kashaya on psoriasis was done by compiling information from classical Ayurveda text, online pediatrics journals, research papers, recommendations and databases like Medline, PubMed etc.
Discussion & Results: All the ingredients of Khadira-Triphaladi Kashaya have the attributes of Kushthaghana (able to cure dermatological afflictions), Dushtavranvishodhana (Cleansing of a vitiated or infected wound), Kandughana (Anti-Pruritic) and have Katu, Tikta and Kashaya Rasa, Laghu, Ruksha Guna, and Ushna Veerya that are helpful in breaking the pathogenesis of Kapha and Pitta dominant Tridoshaja Kustha (~Plaque Psoriasis).
Conclusion: This paper emphasizes the effect of Khadira-Triphaladi Kashaya on plaque psoriasis.
Downloads
References
Edwards CRW, Bouchier IAD, Haslett C, Chilvers ER. Davidson's Principles and Practice of Medicine. 18th ed. USA: ELBS with Churchill Livingstone; 1999. p. 948-52.
World Health Organization. Global Report on Psoriasis. NLM Classification: WR 205; 2016. Available from: https://apps.who.int/iris/handle/10665/204417. [Accessed 2022 Jun 14].
Harden JL, Krueger JG, Bowcock AM. The immunogenetics of psoriasis: a comprehensive review. J Autoimmun. 2015;64:66-73.
Matusiewicz D, Koerber A, Schadendorf D, Wasem J, Neumann A. Childhood psoriasis—an analysis of German health insurance data. Pediatr Dermatol. 2014;31:8-13.
Srikantha Murthy KR. Vagbhata’s Ashtanga Hridaya. Nidana Sthana, Kushta Svithra Krimi Nidanam. Reprint 2019. Varanasi: Chowkhambha Krishnadas Academy; Vol II. p. 136.
Berbi PS, Kokatnur SS. Ayurvedic management of Kitibha Kushta—a case study. J Ayurveda Integr Med Sci. 2022;7(1):390-8. Available from: https://jaims.in/jaims/article/view/1631
Sharma R, Sharma S. Sahasrayogam. Varanasi: Chaukhambha Surabharathi; 2014. p. 286.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 1, p. 97.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 1, p. 162.
Mishra SB, Vaishya SR. Bhavaprakasha Nighantu. Varanasi: Chaukhambha Sanskrit Bhawan; Reprint 2016. p. 837-8.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 1, p. 54.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 2, p. 132.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 1, p. 8.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 1, p. 34.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 1, p. 53.
Tripathi I. Raj Nighantu (Hindi translation). Varanasi: Chaukhamba Bharati Academy; 2003. p. 344.
Jain SK. Ethno-botanical plants of Jaunsar Bawar Mills, Uttar Pradesh, India. Indian J Ethnopharmacol. 1984;12:213-22.
Mandal SC, et al. Pharmacological potentialities of Trichosanthes dioica Roxb. (Cucurbitaceae): an overview. Int J Pharmacogn. 2014;1:422-8.
Tiwari P, et al. Phytochemistry and pharmacology of Tinospora cordifolia: a review. Syst Rev Pharm. 2018;9(1):70-8.
Shah S, Chingale A, Gambhire V. Management of skin disorders in Ayurveda: a review. IRJAY. 2022;5(6):88-91. Available from: https://irjay.com. doi: 10.47223/IRJAY.2022.561.
Anonymous. The Ayurvedic Pharmacopeia of India. Government of India, Ministry of Health and Family Welfare, Dept of ISM & H. New Delhi: The Controller of Publications Civil Lines; 2001. Part I, Vol 1, p. 8.
Gupta A, et al. Pharmacological aspects of Terminalia bellirica. In: Mahdi AA, Abid M, Khan MMAA, Ansari MI, Maheshwari RK, editors. Molecular Biology and Pharmacognosy of Beneficial Plants. Delhi: Lenin Media Private Limited; 2017. p. 52-64.
Said M, Khan BA, Akhtar N, Mahmood T, Rasul A, Irshad H, Hussain H, Khan H, Badshah A. The morphology, extractions, chemical constituents and uses of Terminalia chebula: a review. J Med Plants Res. 2012;6(33):4772-5.
Magotra T, Gupta T. Therapeutic effect of Khadira (Acacia catechu) in Ekakustha (psoriasis). WJPLS. 2020;6(3):152-4.
Sunil MA, Sunitha VS, Radhakrishnan EK, Jyothis M. Immunomodulatory activities of Acacia catechu, a traditional thirst quencher of South India. J Ayurveda Integr Med. 2019;10(3):185-91.
Satpudke S, Pansare T, Khandekar S. Review on Khadira (Cutch tree) (Acacia catechu Willd.) with special reference to Prameha (diabetes). Int J Herb Med. 2020.
Alam G, Singh MP, Singh A. Wound healing potential of some medicinal plants. Int J Pharm Sci Res. 2011;9(1):136-45.
Sharma PV. Gunaratnamala. Edited by Mishra SB, Singh AN. Varanasi: Chaukhamba Sanskrit Bhawan; 2006. p. 226, 431-2.
Srmivasarao D, Jayarraj IA, Jayraaj R, Prabha ML. A study on antioxidant and anti-inflammatory activity of vasicine against lung damage in rats. Indian J Allergy Asthma Immunol. 2006;20:1-7.
Apooshan PG, Sundar K. Anti-ulcer activity of Adhatoda vasica leaves against gastric ulcer in rats. J Glob Pharm Tech. 2011;3(2):7-13.
Rao B, Munjal M, Patnayak A, Loganathan K, Kumar G. Phytochemical composition, antioxidant, antimicrobial, and cytotoxic potential of methanolic extracts of Adhatoda vasica (Acanthaceae). Res J Pharm Tech. 2013;6(9):997-1002.
Bhargava MK, Singh H, Kumar A. Evaluation of Adhatoda vasica as a wound healing agent in buffaloes: clinical, mechanical, and biochemical studies. Indian Vet J. 1988;65(1):33.
Mishra SB, Vaishya SR. Bhavaprakasha Nighantu. Varanasi: Chaukhambha Sanskrit Bhawan; Reprint 2016. p. 837-8.
Bhattacharya S, Haldar PK. Protective role of triterpenoid-enriched extract of Trichosanthes dioica root against experimentally induced pain and inflammation in rodents.
Bhadoriyal SS, Mandoriya N. Immunomodulatory effect of Trichosanthes dioica Roxb. Asian Pac J Trop Biomed. 2012;2:S985-7. doi: 10.1016/S2221-1691(12)60348-7.
Shivhare Y, Singh P, Rajak H, Patil UK, Pawar RS. Antioxidant potential of Trichosanthes dioica Roxb (fruits). Pharmacogn J. 2010;2(6):107-11.
Shivhare Y, Singour PK, Patil UK, Pawar RS. Wound healing potential of methanolic extract of Trichosanthes dioica Roxb (fruits) in rats. J Ethnopharmacol. 2010;127:614-9. doi: 10.1016/j.jep.2009.12.015.
Bhattacharya S, Haldar PK. Trichosanthes dioica roots possess stimulant laxative activity in mice. Nat Prod Res. 2011;PubMed.
Dhanvantari Nighantu, Diwedi BK, editor. Guduchyadi Varga. Varanasi: Chaukhamba Krishnadas Academy; 2008. p. 16.
Pendse VK, Dadhich AP, Mathur PN, Madam MSB. Anti-inflammatory, immunosuppressive, and some related pharmacological actions of the water extract of Neem Giloe (Tinospora cordifolia): a preliminary report. Indian J Pharm. 1977;9:221-4.
Upadhyaya R, Sharma V, Anita KV. Assessment of the multifaceted immune modulatory potential of the aqueous extract of Tinospora cordifolia. Res J Chem Sci. 2011;1:71-9.
Sivakumar V, Rajan MD. Antioxidant effect of Tinospora cordifolia extract in alloxan-induced diabetic rats. Indian J Pharm Sci. 2010;72(6):795-8.
Mishra BS. Bhavprakasa. Varanasi: Chaukhamba Prakashan; 2005.
Chattopadhyay RR. Possible biochemical mode of anti-inflammatory action of Azadirachta indica A. Juss in rats. Indian J Exp Biol. 1998;36(4):418-20.
Sadekar RD, Kolte AY, Barmase BS, Desai VF. Immunopotentiating effects of Azadirachta indica (Neem) dry leaves powder in broilers, naturally infected with IBD virus. Indian J Exp Biol. 1998;36(11):1151-3.
Hossain MA, Al-Toubi WAS, Weli AM, Al-Riyami QA, Al-Sabahi JN. Identification and characterization of chemical compounds in different crude extracts from leaves of Omani Neem. J Taibah Univ Sci. 2013;7(4):181-8.
Barua CC, Talukdar A, Barua AG, Chakraborty A, Sarma RK, Bora RS. Evaluation of the wound healing activity of methanolic extract of Azadirachta indica (Nimba) and Tinospora cordifolia (Guduchi) in rats. Pharmacologyonline. 2010;1:70-7.
Sharma RK, Dash B. Caraka Samhita, Volume II. Varanasi: Chowkhamba Sanskrit Series; 1998.
Sivasankar S, Lavanya R, Brindha P, Angayarkanni N. Aqueous and alcoholic extracts of Triphala and their active compounds chebulagic acid and chebulinic acid prevented epithelial to mesenchymal transition in retinal pigment epithelial cells by inhibiting SMAD-3 phosphorylation. PLoS One. 2015 Mar 20;10(3):e0120512.
Rasool M, Sabina EP. Anti-inflammatory effect of the Indian Ayurvedic herbal formulation Triphala on adjuvant-induced arthritis in mice. Phytother Res. 2007 Sep;21(9):889-94.
Srikumar R, Parthasarathy NJ, Rathinasamy, Devi RS. Immunomodulatory activity of Triphala on neutrophil functions. Biol Pharm Bull. 2005;28(8):1398-403.
Vani T, Rajani M, Sarkar S, Shishoo CJ. Antioxidant properties of the Ayurvedic formulation Triphala and its constituents. Pharm Biol. 1997;35(5):313-7.
Mahalakshmi K, Prabhakar J, Sukumaran VG. Antibacterial activity of Triphala, GTP, and curcumin on Enterococcus faecalis. Biomedicine. 2006;26(3-4):43-6.
Revathi S, Gopal V, Jeyabalan G. Acute toxicity and in vivo laxative studies of Triphala extract in experimental animals. J Drug Deliv Ther. 2019 Jul 15;9(4):341-7.
Tripathi B. Caraka Samhita, Sutra Sthana. Varanasi: Chaukhamba Subharati Prakashan; 2014. Chapter 26. p. 484.
Gaur BL. Ayushakamiya, Sutrasthana. Ashtanga Hridayam, Samvarta commentary. Vol 1. Varanasi: Chaukhamba Orientalia; 2007. 1/26:13.
Shastri A. Sushruta Samhita, Sutra Sthana. Varanasi: Chaukhamba Sanskrit Sansthan; 2017. Chapter 46. p. 289.
Vagbhata. Ashtanga Hridayam. Gupta AK, editor. Sutra Sthana. Varanasi: Chaukhamba Prakashan; 2009. Chapter 9. p. 107.
Tripathi B. Caraka Samhita, Vyodani Hindi Commentary. Sutra Sthana. Varanasi: Chaukhamba Subharati Prakashan; 2014. Chapter 26. Sloka 59-62.
Shastri A. Sushruta Samhita, Sutra Sthana. Varanasi: Chaukhamba Sanskrit Sansthan; 2017. Chapter 41. Sloka 15. p. 289.
Bhati A, Yadav CR, Gurao R. Scope of Ayurveda in the management of Kushtha (skin diseases). IRJAY. 2024;7(4):45-9.
Satpudke S, Pansare T, Khandekar S. Review on Khadira (Acacia catechu Willd.) with special reference to Prameha (diabetes). Int J Herb Med. 2020.
Franco P, Potenza I, Moretto F, Segantin M, Grosso M, Lombardo A, Taricco D, Vallario P, Filippi AR, Rampino M, Ricardi U. Hypericum perforatum and Nimba oil for the management of acute skin toxicity in head and neck cancer patients undergoing radiation or chemo-radiation: a single-arm prospective observational study. Published online 2014 Dec 29.