Women Mental Health w.s.r. to Premenstrual Syndrome - An Online Survey
Abstract
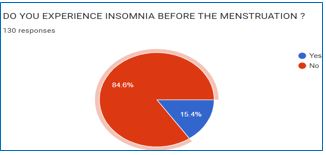
Introduction: Premenstrual syndrome (PMS) is a psycho neuroendocrine disorder of unknown aetiology. Prevalence of PMS is 47.8% in world-wide and in India it is 43%. It is mainly affecting mental health of the women, and quality of life of the women so this research was planned to explore the severity of the premenstrual syndrome and to evaluate the impact of PMS on Women mental health. Materials & Methods: Among 160 females, 130 females enrolled in the study based on criteria. The data was collected through Google form which was prepared based on PSST (premenstrual Symptom Screening Tool) Scale. Results: One hundred and twenty-two participants reported at least three somatic and two affective symptoms. 34.7% participants mentioned that PMS affects their quality of life. 30.3% participants reported mild, 24.6% female reported moderate, 10.7% reported severe and 7.4 % stated very severe. PMS significantly having relation with occupation, stress, and physical exercise. 57% participants reported that they are stressed due to any personal/ occupational issues. The participants who are doing regular exercise/ yoga are having less severity of symptoms compared to other participants. Discussion: This study reveals that PMS is common in almost all females but degree of severity differs. It affects both mental and physical health and also quality of life of the women. By this study additional thing we found that women who practice yoga, Pranayama, any physical exercise have less severity of premenstrual symptoms.
Downloads
References
Konar. H, editor. Text book of Gynecology. 6th ed. New Delhi: Jaypee Brothers; 2013. p.182.
Direkvand-Moghadam A, Sayehmiri K, Delpisheh A, Kaikhavandi S. Epidemiology of premenstrual syndrome (PMS)-a systematic review and meta-analysis study. Journal of clinical and diagnostic research: JCDR. 2014 Feb;8(2):106.
Dutta A, Sharma A. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in India: A systematic review and meta-analysis. Health Promotion Perspectives. 2021;11(2):161.
Yonkers KA, O'Brien PM, Eriksson E. Premenstrual syndrome: Lancet. 2008 Apr 5;371(9619):1200-10. doi: 10.1016/S0140-6736(08)60527-9. PMID: 18395582; PMCID: PMC3118460.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Premenstrual syndrome: Treatment for PMS. [Updated 2017 Jun 14]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279264/
Marjoribanks_J, Brown_J, O'Brien PMS, Wyatt_K. Selective serotonin reuptake inhibitors for premenstrual syndrome: Intervention review. Cochrane Database of Systematic Reviews. 2013; Issue 6. Art. No.: CD001396. DOI:10.1002/14651858.CD001396.pub3.
Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011 Jul;4(2):49-54. doi: 10.4103/0973-6131.85485. PMID: 22022122; PMCID: PMC3193654.
Vaghela N, Mishra D, Sheth M, Dani VB. To compare the effects of aerobic exercise and yoga on Premenstrual syndrome. J Educ Health Promot. 2019 Oct 24; 8:199. doi: 10.4103/jehp.jehp_50_19. PMID: 31867375; PMCID: PMC6852652.
Bharati M. Comparing the Effects of Yoga & Oral Calcium Administration in Alleviating Symptoms of Premenstrual Syndrome in Medical Undergraduates. J Caring Sci. 2016 Sep 1;5(3):179-185. doi:10.15171/jcs.2016.019
Steiner M, Peer M, Palova E, Freeman EW, Macdougall M, Soares CN. The Premenstrual Symptoms Screening Tool revised for adolescents (PSST-A): prevalence of severe PMS and premenstrual dysphoric disorder in adolescents. Archives of women's mental health. 2011 Feb;14(1):77-81.
Shah RS, Christian DS. Association of socio-demographic, dietary and lifestyle factors with Premenstrual Syndrome (PMS) among undergraduate medical students of a tertiary care institute in Ahmedabad, Gujarat. Journal of Family Medicine and Primary Care. 2020 Nov;9(11):5719.
Hofmeister S, Bodden S. Premenstrual syndrome and premenstrual dysphoric disorder. American family physician. 2016 Aug 1;94(3):236-40.
National Health Portal [Internet].India: Premenstrual Syndrome;2016 Oct 14[cited 2021 July 8];[about 1 screen].Available from:https://www.nhp.gov.in/disease/gynaecology-andobstetrics/premenstrual-syndrome
Kamat SV, Nimbalkar A, Phatak AG, Nimbalkar SM. Premenstrual syndrome in Anand District, Gujarat: A cross-sectional survey. Journal of Family Medicine and Primary Care. 2019 Feb;8(2):640.
Heinemann LA, Do Minh T, Filonenko A, Uhl-Hochgräber K. Explorative evaluation of the impact of severe premenstrual disorders on work absenteeism and productivity. Women's Health Issues. 2010 Jan 1;20(1):58-65.
Jahromi BN, Pakmehr S, Hagh-Shenas H. Work stress, premenstrual syndrome and dysphoric disorder: Are there any associations?. Iranian red crescent medical journal. 2011 Mar;13(3):199.